Last year made it abundantly clear that infection prevention and control in hospitals is paramount to slow the COVID-19 pandemic and maintain a surplus of unoccupied hospital beds. While COVID-19 is at the top of our collective minds, other looming threats such as MRSA, and thousands more documented and unknown zoonotic diseases, mean it’s imperative for hospitals to get a handle on infection control protocols now, in order to prepare for whatever the future brings.
Lean Design is a process-driven approach that examines the layout, flow, processes and protocols of a hospital, focusing on identifying and eliminating bottlenecks and areas of waste. For infection control, the application of Lean Design helps ensure processes for staff, patients and materials that encounter potential pathogens have as few opportunities as possible for cross-contamination with those that do not.
For everything that moves within a healthcare facility, there is a process for that item to arrive at its destination — be it a roll of toilet paper, a surgical scalpel, personal protective equipment, staff or patients. Lean Design looks deeply to refine each process by minimizing unnecessary movement and waste, which inherently prevents cross-contamination.
Designers who apply Lean Design focus on efficiency-centric metrics, such as minimizing the number of steps taken, eliminating the search for supplies and avoiding interruptions. Since every facility has different needs, designers should assess the layout and processes of a given facility during operations to identify problems and tailor specific solutions.
How COVID confusion creates contamination
When COVID-19 first hit, many hospitals had to change the function of their units or rooms to accommodate an influx of infectious patients. Since the symptoms require multi-disciplinary intervention, staff from multiple departments had to converge in unfamiliar pods.
Many had a hard time adjusting to new layouts and knowing where to quickly find important supplies and resources. This not only increased staff anxiety, but also made their jobs harder. The unfamiliarity of their environment also increased the potential number of times contaminated personnel and equipment crossed paths with uncontaminated personnel and equipment, threatening the hospital’s overall ability to contain the virus.
Eliminating cross-department confusion with signage
Cross-department confusion could be one of the biggest contributing factors to challenge infection control in a hospital during a surge event. The ideal solution is to employ Lean Design principles to create paths where clean and contaminated processes are always separate, while utilizing strategies that reduce staff confusion.
Let’s explore a hypothetical scenario in which a respiratory therapist is transferred on short notice to a pod that was recently repurposed into a COVID-19 unit. Upon arrival, they might not know where the proper receptacle to dispose of soiled supplies is located, creating a scenario where they could overlap clean processes with contaminated materials.
This would compromise the integrity of the unit and the safety of its occupants, who could go on to unknowingly track the contaminant through other areas of the hospital. To make matters worse, the further the respiratory therapist travels to find out what they need to know, the wider the contamination will spread. Additionally, they will interrupt the processes other staff members are engaged in, creating distractions in an environment where everyone must be focused on performing their tasks as safely as possible.
Using Lean Design principles to evaluate the process of materials movement in this particular scenario, excess motion of contaminated materials and interruptions to staff workflow are identified as waste. One effective solution to eliminate cross-department confusion would be to develop a standardized signage system with highly visible, consistent, simple and bold graphics hospital-wide.
A hospital could use red signs with X’s to show where soiled material is disposed of, purple signs with triangles for the environmental services closet and green signs with circles for clean supplies. No matter what department staff members work in, they’ll all be on the same page.
Standardized signage keeps people from having to ask questions, regardless of where they are in the hospital, which minimizes interruptions, as well as the overlap of clean and contaminated materials and staff members.
Controlling infection with autonomous containment zones
When dealing with a pandemic response event, it’s crucial to establish autonomous containment zones where staff are “locked in” for the duration of their shift. This limits the movement of people, equipment and supplies from inside the contaminated area to the rest of the hospital.
There are two waste-elimination strategies from Lean Design evaluation that can be used to establish autonomous containment zones: containment and autonomy.
Containment
The efficacy of containment zones relies on the key strategy that once someone enters, they are there to stay. In this case, the movement of personnel is the process to be refined. Inside the containment zone, strict safety protocols must also be followed, but the first priority of those who enter should be to separate from other departments and staff in order to maintain the integrity of the rest of the facility.
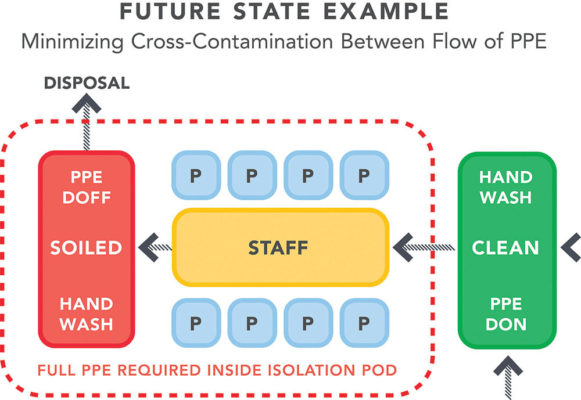
By evaluating the flow of staff and PPE through an area of contamination, process review suggests the best way for people and supplies to enter and exit the containment zone is to do so in a one-way flow pattern. When they enter, they do so through the “clean” side, where they can don new PPE and wash their hands before entering the “bubble.”
People then exit through the “soiled” side, depositing used PPE in a secure disposal bin within the containment zone on the way out to avoid contaminating the rest of the hospital. The exit area should have the necessary utilities for staff to decontaminate themselves before heading home. While repurposed spaces may not be able to accommodate all of these measures, the ideal exit area of a containment zone would include:
- Soiled materials deposits situated in an area that allows for direct removal from the hospital
- Decontamination shower with a separate exit, if space allows
- Hand-washing station
Autonomy
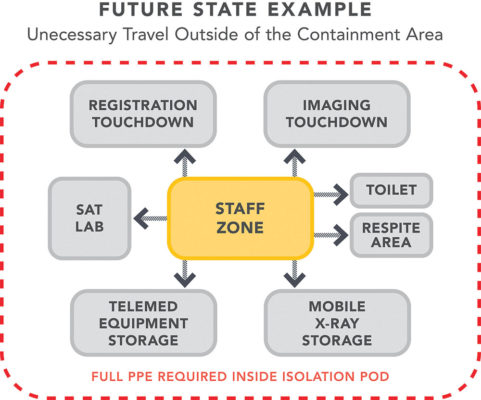
For staff to remain within the zone for the duration of their shift, it must be more than just a unit with space for sick patients. The entirety of the workflow for staff members must be evaluated and understood to identify what other tasks and activities beyond patient care influence their movement. In addition to caring for patients, they’ll be taking breaks, eating meals and fielding calls from loved ones.
Containment zones should be a bubble containing everything staff and patients need. That includes medical equipment and supplies in addition to staff support spaces.
COVID-19 has put a spotlight on the extraordinary stress healthcare workers go through while treating patients hospitalized with a brand-new virus. Being essentially locked into a bubble with infectious patients could certainly increase that existential stress healthcare workers carry, so measures must be taken to protect their mental health.
Staff respite spaces should be incorporated within containment zones to seamlessly support staff mental health without disrupting an efficient work or infection control process. These are places where they can privately take a moment to reflect, make a call home or enjoy a meal.
These spaces should have a small variety of comfortable seating, adjustable lighting, acoustical privacy to create a sense of being off-stage from the hospital floor, as well as Wi-Fi connectivity so staff can browse the internet or communicate with their families or mental health professionals.
COVID-19 has cemented the fact that infection control is a top priority in keeping the healthcare system above water, especially during a pandemic. With Lean Design infection control protocols, healthcare workers will be prepared to protect themselves and their patients, without having to worry about bringing dangerous diseases home to their loved ones.



