Evaluating similarities, differences between American and Chinese hospitals to create positive outcomes
Providing near-universal healthcare to a population of more than 1.4 billion citizens is no easy task, but that’s exactly what the Chinese government has set out to accomplish. One of the many steps to achieve such an elaborate goal was to permit private payers and providers to address the increasing needs of higher-income patients.
Take the Taikang Insurance Group: founded in 1996, this firm has grown significantly since its inception and is now one of the largest life insurers by premium income in China. In 2015, the Taikang Group vertically integrated into the provider side and acquired an 80 percent stake in Nanjing Drum Tower Hospital for approximately $767 million. Similar to an integrated healthcare system in America, the Taikang Group focuses on the continuum of care, health plan offerings, preventive care, inpatient and outpatient care and more.
The Taikang Group recognized the need for process and design improvements within the Drum Tower Hospital’s emergency department due to an anticipated patient volume increase by 300 percent over the next few years. The hospital’s executive president expressed interest in increasing the ED’s utilization rate to improve clinical outcomes and patient satisfaction. The president asked for optimal improvements with minimal daily interruptions to operations and physical layout.
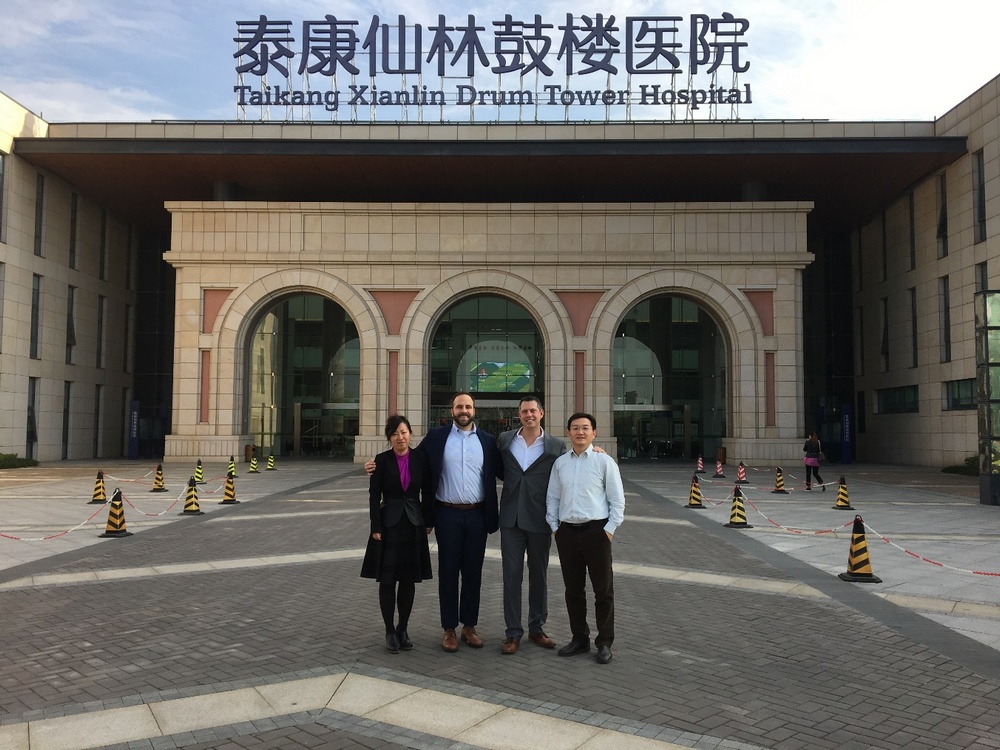
The Taikang Group and Drum Tower Hospital partnered with the Operational Excellence Group at CallisonRTKL. The goal was to improve operational efficiency by the elimination of waste and to complete simulation modeling analysis for multiple scenarios. The CRTKL OpEX group traveled to Nanjing, China and visited the hospital, where they presented at a strategy kick-off meeting. Over the course of the week, the group interviewed frontline staff and leadership and recorded time observations, patient volume and arrival patterns.

After one week of observations, the OpEX team noticed similarities and differences between American hospitals and the Chinese Drum Tower. In America, hospitals tend to promote the idea that every patient will be given superb treatment. However, in China, the Drum Tower Hospital dedicates an entire patient wing for only VIP patients. In fact, for an additional cost, Drum Tower patients can access this wing that includes 20 hotel-like suites, meditation areas and a dedicated food service. While these were only the noticeable upgrades, this comes with vast amounts of underutilized space throughout the building.
For example, upon entering the large atrium that welcomes patients and family members, the group made note of the numerous escalators that were barely used, copious empty waiting areas and several long, dark hallways that were dead ends. Most American hospitals can’t afford this type of empty and underutilized space.
In America, it’s common for EDs to have dedicated staff for patient transportation and to relieve clinical staff from non-clinical duties. American healthcare providers walk from room to room to check on their patients, while in Chinese EDs, the opposite occurs. Chinese healthcare providers remain stationary in an exam room-like setting, waiting for the continuous revolving door of patients to enter and exit. Upon exiting from a provider consultation, patients are expected to pay for services rendered each time during the same visit, rather than a cumulative final bill after discharge.
Following the OpEX team’s visit to China, the group began to perform advanced data analysis, process improvement and simulation modeling for multiple processes and facility scenarios. Bi-weekly virtual meetings were held for several months with the hospital’s facility management, executive leadership, ED, clinical leadership, the Taikang Group’s leadership and in-house architects to collaboratively discuss the group’s findings. These working meetings were imperative since the outcomes would determine the project’s success.
For project implementation success, the OpEX team needed to prepare and motivate everyone, involve as many hospital leadership and front-line employees as possible and share and manage the final outcome expectations. During this discovery phase of the project, the goal was not only to plan and design the space, but to understand how the design impacts room utilization, capacity, throughput, patient satisfaction, length of stay, patient waiting times and value added vs. non-value-added activities. In addition to the ED’s key performance metrics, the OpEX team began to compare construction costs, operational disruptions, patient capacity and, most importantly, a financial assessment for every scenario.

One of the first upgrades within the ED was improving the payment process. Through Lean Six-Sigma tools—such as process maps, spaghetti diagrams, discrete-event simulation modeling and value stream mapping—the OpEX group highlighted the waste from making patients pay for every service throughout one visit. By reducing the number of payment steps, on average, every patient would be required to walk 50 meters less per visit. With this paradigm shift, moving toward a patient-centric experience altered the group’s mindset and drove the future design of the ED.
The next upgrade included an in-depth analysis of each exam room utilization rate, by specialty, to simulate modeling future patient volumes. The group’s findings concluded that the internal medicine exam rooms’ utilization rate averaged approximately 85 percent and reached 95 percent almost daily. The OpEX group suggested to create one flexible room which would treat ophthalmology patients during non-peak hours and internal medicine patients during peak hours, and then an additional permanent internal medicine exam room. A final hybrid-layout option included combining the triage and registration process, adding two additional exam rooms, reassigning an ENT exam room for internal medicine, improving the payment process and changing the triage and registration area from one-sided to two-sided.
Through advanced data analysis, direct observation, staff interviews and simulation modeling, the group carefully evaluated five different options for improvement to process and layout. Each option was evaluated against a future forecasted patient volume and, after meeting with the hospital and the Taikang Group leadership to discuss project findings, a final hybrid layout option was chosen. This hybrid layout combined triage registration space in the ED, along with an enhanced process, which optimized results in a new ED that can accommodate a 40 percent increase in patient volume—equating to additional revenue of approximately $3.5 million per year.
This project showcases the importance of Lean and Six-Sigma methodologies, ensuring collaborative communication and consensus building, while creating an environment where the best ideas win. By applying Lean and Six-Sigma methodologies to the beginning of the project, the group was more prepared to define processes and eliminate waste and variation so that, collectively, they could create the best experience for the patient and their families. In addition, the integrated project team were able to simulate the current process to better understand how these practices can impact various performance metrics within the ED, and to assist and support executive decisions.