The minute health systems started shutting down services at the start of the COVID-19 pandemic, reality hit that something was broken. It was more than the supply chain, which buckled under a 17-fold increase in demand for such things as facemasks and gowns at a time when organizations only kept 15-30 days of supplies on hand.
It was greater than a need for more ICU beds and negative pressure rooms available to treat infected patients when population health strategies were designed to mitigate the need for people to be hospitalized.
It went beyond actual surge capacity, as the demands on staffing both put care team members at risk of contracting the virus, as well as overstretching nurses, doctors and therapists with few resources for reprieve.

It was everything: from traffic flow to infection control, technology to mechanical capacity. The strain of closed clinics and operating rooms proved to be greater than many had anticipated and, coupled with overtime for staff, as well as expenses for quick room conversions and price increases for equipment, financial losses are expected to exceed $323 billion dollars in 2020, according to the American Hospital Association.
The situation has elicited one large question: “How did we get here?”
While an understatement, COVID-19’s sweep across the nation exposed a deficiency in the quest for efficiency and better cost management. The physical and operational systems designed to serve our communities’ health needs have fallen short in meeting those needs when the demand surges.
Leading to the current state was a planning process that put efficiency and patient satisfaction at the center of the process. Missing from that was the inclusion of resiliency, both operationally and financially, in order to navigate scenarios that force organizations to deviate from normal operations.
Most campuses and facilities have been programmed through a master planning process, a practice that usually relies on observed trends to forecast a probable future. What the pandemic has shown is that the scenario under which the plans are crafted focus on a desirable future, one predicated that the future will be similar to the past. More than planning for a worst-case scenario, there’s a recognition that the planning process needs to evolve to consider all the scenarios that could impact healthcare operations. Scenario planning puts the integrity and resiliency of an organization’s operations at the center of the planning process.
Redefining resiliency
Resiliency in the built environment has traditionally been defined by a building’s ability to survive an adverse event, whether that’s an F2 tornado, a 500-year flooding event, a category 3 hurricane or an earthquake of a varying magnitude. Regionally oriented, designing for resiliency has been more a physical exercise related to downtime and recoverability.
Resilience, though, is more than a physical state. It’s also an operational state. Gartner, a business consultancy, defines operational resilience as a “set of techniques that allow people, processes and informational systems to adapt to changing patterns. It is the ability to alter operations in the face of changing business conditions.” Economic studies of operational resilience break down the term into two components: disruption absorption dimension and recoverability dimension—the first being defined as the ability of an organization to maintain structure and normal operations in the face of disruptions, and the latter as the ability of an organization to restore operations to a prior normal level of performance after being disrupted. Applying this concept to healthcare, a hospital facility’s ability to withstand a 175-mile-per-hour tornado would fall under recoverability, while the organization’s ability to maintain continuous operations coming out of such an event would fall under disruption absorption.
Under the Triple Aim for healthcare developed by the Institute of Healthcare Improvement, the design approach to healthcare facilities and campuses seeks to optimize a health system’s performance by simultaneously pursuing the improvement of the patient experience, the improvement of the health population and a reduction in healthcare cost. Missing from this aim has been the discussion of resiliency. As the ramifications of the coronavirus on the integrity of organizational operations are more fully understood, it brings into clearer focus a need to consider resiliency within the Triple Aim framework, evaluating how the needs of the broad community can be met, while absorbing the disruption presented by a pandemic or any scenario which a healthcare organization would have to absorb.
The 14-story, 830,000-square-foot patient tower opened in 2012 by Rush Medical Center, located in Chicago, Illinois, demonstrates this approach, designed from the experience of the Sept. 11 attacks and anthrax scares in 2001. Entire floor conversions designed for negative pressure airflow, ambulance bays that could act as triage units and decontamination units and an atrium that could flex to an emergency room for noninfectious patients with access to gases, oxygen and power in the atrium columns, allows Rush to expand bed capacity by 133%.
When COVID-19 hit the Chicagoland area, Rush Medical Centered pivoted to surge capacity in 11 days, complemented by the Army Corps of Engineers’ conversion of McCormick Place into a 3,000-bed alternative care site.
As the Rush Medical Center case study shows, the solutions go beyond facilities, while also putting the physical infrastructure at the heart of the planning. The community, enterprise and operations of a healthcare organization need to be factored to achieve resiliency. Operationally resilient enterprises have the organizational competencies to ramp up or slow down operations in a way that enables quick and local process modification. Similarly, healthcare organizations need to alter in the face of changing scenarios, one that is dynamic to continuously improve the patient experience, population health and costs of care.
From master planning to scenario planning through resiliency
There is a need to evolve the traditional master campus planning process to present tangible ways healthcare organizations can achieve resiliency in their facility under normal and extreme circumstances. Master planning as it’s been practiced usually relies on observed trends to forecast a probable future. While data informed, it is a consensus-driven event that focuses on a desirable future.
The cracks exposed in the practice is an assumption baked into the predictive modeling – that the future will be similar to the past. Visionary and aspirational, master planning has assumed a stable environment, an assumption that overlooks how unplanned events can strain operations, not just impact facilities.
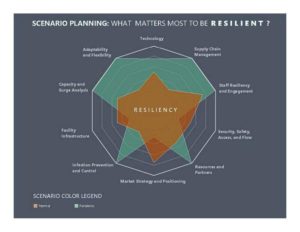
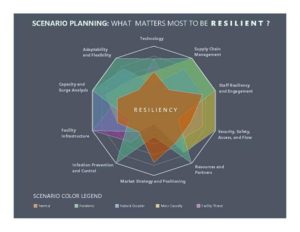
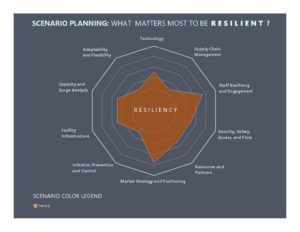 Scenario planning is more dynamic, allowing an organization to see their future through a set of events that could impact their operations (see Figure 1). Rather than focusing on what is desirable, scenario planning explores how operations can deviate from a defined normal through the uncertain: a natural event, a mass casualty event, a physical or cyber-attack on a facility or a pandemic. While not high-probability events, these scenarios represent a strain on an organization’s resources.
Scenario planning is more dynamic, allowing an organization to see their future through a set of events that could impact their operations (see Figure 1). Rather than focusing on what is desirable, scenario planning explores how operations can deviate from a defined normal through the uncertain: a natural event, a mass casualty event, a physical or cyber-attack on a facility or a pandemic. While not high-probability events, these scenarios represent a strain on an organization’s resources.
Scenario planning puts the integrity of organizational operations at the center of the planning process, giving organizations the ability to understand the possible effects these events may have on their personnel, supplies and facilities. Like master planning, it is an interactive process, but it is structured to help organizations better understand and identify future facility and operational needs under a variety of conditions, revealing opportunities to shape their campuses and facilities for both normal and abnormal operations.
Facilities and infrastructure are then designed for disruption absorption – alternative care sites, alternative care delivery methods, flexible mechanical systems, adaptable spaces, alternative traffic flows, as well as support for staff wellness under unrelenting stress. By creating a dialogue between all the various parts of an organization, a plan is shaped to help organizations maintain the integrity of their operations through adversity.
 For many healthcare organizations, both rural and urban, telemedicine has been the most visible example of such planning and deployment. As clinics limited access during the pandemic, both to mitigate infection spread and preserve needed PPE supplies for emergency and inpatient personnel, organizations immediately turned to telemedicine as a way to serve patients and maintain revenue. Deployment required coordination between clinicians, IT, marketing and facilities to create a program that could successfully meet the needs of patients who can’t or don’t want to come in for a physical visit.
For many healthcare organizations, both rural and urban, telemedicine has been the most visible example of such planning and deployment. As clinics limited access during the pandemic, both to mitigate infection spread and preserve needed PPE supplies for emergency and inpatient personnel, organizations immediately turned to telemedicine as a way to serve patients and maintain revenue. Deployment required coordination between clinicians, IT, marketing and facilities to create a program that could successfully meet the needs of patients who can’t or don’t want to come in for a physical visit.
As Tom Clark, chief strategy officer of Avera Health, noted, COVID-19 has shown organizations what the value of telemedicine is even post-pandemic to meeting patients where they are, expanding services and delivering needed care in the most remote of regions.
For rural hospitals, especially, this could be a resiliency blueprint to surviving adverse scenarios when, even in more normal times, margins are already thin if not non-existent. By bringing other parts of the organization to the table who may not have previously participated in master planning processes, organizations can broaden the discussion to incorporate all the facets of operations that could be impacted and respond to scenarios that deviate from normal.
 Surges with the pandemic continue to challenge hospitals and health systems even as more is learned about the treatment of the disease. While living in the moment and pivoting resources to respond to community needs, such as converting ambulance bays into drive-thru testing centers, organizations are also asking, “How do we move forward?”
Surges with the pandemic continue to challenge hospitals and health systems even as more is learned about the treatment of the disease. While living in the moment and pivoting resources to respond to community needs, such as converting ambulance bays into drive-thru testing centers, organizations are also asking, “How do we move forward?”
Planning for a post-pandemic world, there is a recognition that scenarios forcing organizations into crisis operations – biohazard and chemical incidents, mass casualty events, floods and tornadoes, pandemics or even ransomware attacks – are no longer 100-year events. They’ve all occurred in some capacity within the past 15 years in all areas of the nation.
The flood of need for hospitalization in the pandemic isn’t an indictment that the previous pursuits were wrong. Rather, in exposing the gaps in healthcare operations, the pandemic has revealed the need to evolve our planning approaches so that the physical demands of a health crisis don’t threaten an organization’s ability to meet the demands for community health, overall.




