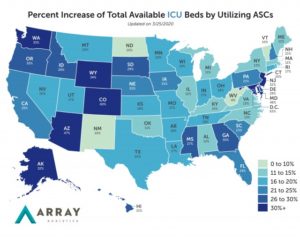
A new model by Array Analytics projects the potential increase in bed capacity if health systems leverage ambulatory surgery centers to boost bed availability. Breaking down potential ASC surge capacity within each hospital referral region and state, the model projects that employing ASCs will increase the national potential ICU bed supply by 21% and med-surg bed supply by 8%.
Healthcare strategists have proposed using ASCs to house non-COVID-19 cases, increase overall bed availability in hospitals or designate pure COVID-19 treatment hospitals. The company’s analyses reveal that while ASCs can provide additional capacity for the healthcare system, they only afford a few days’ additional capacity in most markets. It estimates the number of ICU and med-surg bed equivalents available at ASCs based on the number of operating rooms, anesthesia machines and the prevalence of phase one and phase two recovery bays.
The surge capacity alternative space model builds on CMS data, pivotal data and Array Advisors’ ICU bed demand model that projects ICU bed capacity against local and national supply. The ICU model’s latest projections (not yet published) underscore the urgent need for solutions that expand hospital capacity.
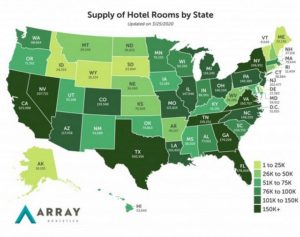
Health systems will use a prioritized response as they choose overflow strategies. First, health systems will take immediate measures to increase capacity at each hospital facility, such as those proposed in this surge capacity planning tool. However, even with hospital capacity optimized, it is projected that space requirements will quickly outweigh available resources. Second, health systems will evaluate the use of ASCs, which already house the space, personnel and equipment needed for COVID-19 treatment or for the treatment of non-COVID-19, non-elective patients. Third, health systems will assess alternative locations, such as hotels, convention centers and vacant large retail spaces.
The company has included hospitality supply by state and HHR in its model, with information provided by STR. Hotels offer robust technology platforms, proximity to densely populated areas and a planning and space model that make them ideal for either isolating mildly ill people who have been diagnosed with COVID-19, or housing those who have been exposed and should be quarantined.
Recent changes in telehealth delivery and reimbursement regulations remove some barriers to deploying healthcare infrastructures broadly in unconventional healthcare spaces. Telemedicine could potentially be used to provide care if it buttressed by onsite support for patients that become critical (5% of total cases) and robust transfer protocols.