Strategies to future-proof hospitals against obsolescence
The Hill-Burton Act was enacted in 1946 to increase the supply of hospital beds by providing construction grants to nonprofit entities. It was very successful: Between 1947 and, when funding ended in 1970, about a half-million additional hospital beds were added (http://igpa.uillinois.edu/). What the act didn’t, and couldn’t, anticipate were medical advances that slowly rendered the Hill-Burton version of the inpatient hospital virtually obsolete.
Hill-Burton era hospitals were not designed to adapt because there wasn’t much to adapt to
Hill-Burton hospitals were a major improvement over what existed: cottage hospitals and facilities with open wards, for example. Many of the new hospitals offered double-bedded rooms and better operating and diagnostic facilities. These hospitals served their purpose well but didn’t lend themselves easily to retrofitting. Most chose to add onto existing facilities to gain more square footage and utility. Cost was no object, and adaptability was not a design feature: we just kept making more Hill-Burton-like facilities.
The 70s, however, began an era of medical technology advances that slowly made these hospitals obsolete. The first free-standing ambulatory surgery center opened in 1970 (www.ascassociation.org), at the very end of the Hill-Burton era and, while many hospital surgical departments adapted to this change and grew their outpatient surgery business, the inpatient admissions they lost were never recovered.
We are now in an era of rapid change, more is coming
Today, technological and financial pressures are shuttering inpatient units, closing hospitals and, in many markets, consolidating inpatient care into academic medical centers. And these old facilities are not easily adaptable. Consider that:
- Single-bedded rooms, deemed better at preventing the spread of infection and offering a better experience, are practically a requirement.
- The migration of inpatient surgery to the outpatient setting has accelerated to the point that even a lot of outpatient surgery is now office-based.
- The need for a physician to go to the community hospital to see patients, get information or even collegiality doesn’t exist. Much better and more accurate medical knowledge is available online and increasingly built into the electronic health record, hospitalists see inpatients and collegiality is built around organizations that manage at-risk contracts.
- Machine intelligence and robotic systems will take over more and more routine logistical functions in hospitals.
- Knowledge systems like IBM’s Watson will perform more diagnostic work.
- Active and passive clinical robotics will quicken inpatient and outpatient operating and recovery times, rendering overnight stays, and even the less-than-24-hour stay, unnecessary.
- Super urgent care and free-standing emergency rooms are replacing many of the functions of the traditional hospital-based emergency department.
- Even research and training are not immune. Dry research is superseding wet research. As the new virtual world of healthcare becomes a reality, researchers will spend more time on the data generated from personalized sensors and computer modeling than on traditional animal studies. Research hospitals will struggle to adapt. We will need to produce more medical data scientists, and their residencies won’t take place in a hospital.
Inpatient hospitals aren’t going away
Even so, we still need hospitals with beds:
- Individual traumas will happen, requiring hospitalization
- Major emergencies and disasters will occur, requiring facilities to treat people
- There will be very sick people with multiple diseases that need intensive care
- Treating people with highly infectious diseases requires isolation
- Given the advances in healthcare nanotech, future hospitals will need to have a higher level of bio-containment than ever before to ensure this nanotech doesn’t leak into the environment
- Almost all births will continue to be in hospitals.
Let’s build obsolescence into our new healthcare facilities
If we must still build hospitals, they must be adaptable and able to anticipate their own obsolescence with the infrastructure to adapt and change rapidly and economically. By adaptable, this doesn’t mean designing facilities that can be added onto in a coherent way—we know how to do that. It means designing facilities where whole units, departments or functions can be easily replaced in situ without additional square footage.
We have advanced architectural, engineering and construction techniques that enable pre-fabrication and modularization. Operating and procedural rooms of all types can be assembled and reassembled easily now with no loss of infection control and utility. Wireless technology further enables this. We can take lessons from the military and how they have containerized just about everything, including patient beds and operating rooms. We need to think more about plug-and-play units, a decade at a time, housed in a shell built for the long term.
Design adaptability, flexibility in room utilization and facility design
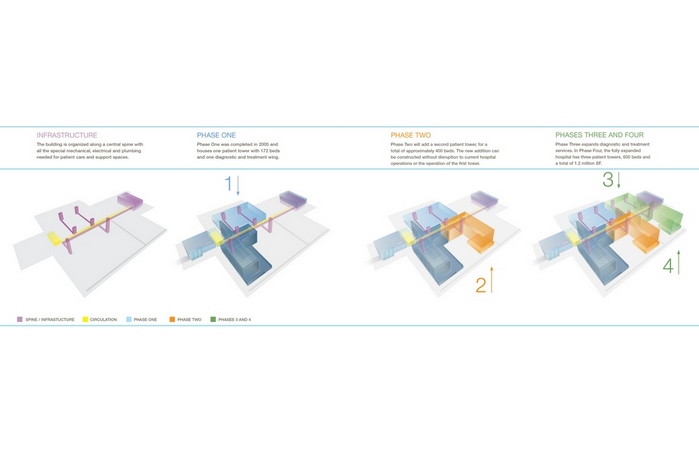
We need to move past the traditional view of a building as a static object, and instead explore opportunities for designing a building as an open-ended framework of integrated components. By developing a component logic that is highly standardized, demountable and multi-functional, key areas within the framework can be repurposed, reconfigured or replaced as requirements evolve. This reduces the likelihood of future disruption and waste and increases the potential lifespan of the entire project—a breakthrough in terms of lifecycle sustainability.
Elements of this integrated infrastructure strategy might include:
- Permanent infrastructure elements, such as public circulation (horizontal and vertical), mechanical and electrical service areas and shafts or risers, located at the periphery of large and regular floor plates that are free of major obstructions
- Open floorplate areas based on uniform modules of space suited for many different functions
- Universal rooms sized and configured to accommodate a range of uses
- Modular and/or movable casework and systems furniture
Bad adaptations serve no one well, neither patients, nor visitors nor the caregivers who work in the hospital. An adaptable and flexible hospital can future-proof itself against obsolescence, changing as healthcare changes and organic to the requirements necessary at any particular point in time.