Subscribe Now
Changing the Game
By Stan Chiu
Rise of the collaborative medical center model
The healthcare industry in the U.S. is changing and transforming at a rapid pace that many don’t even realize. This is due in part to the introduction of the latest wearable technology from companies like Apple and government legislature like the healthcare law – but it doesn’t stop there. There is one trend that stands out to transform the way we receive healthcare services. It’s centered on the collaborative medical center model.
The typical healthcare model is physician-centric and involves usually one encounter per visit. For example, a patient being treated for diabetes would be heavily relied on to manage their own care among all of the different specialists. One appointment would be for an endocrinologist, another to see a nutritionist and another to see a pharmacist. There would be nothing connecting these specialists together to consider the best option for the patient, resulting in the patient being the care coordinator for their own treatment.
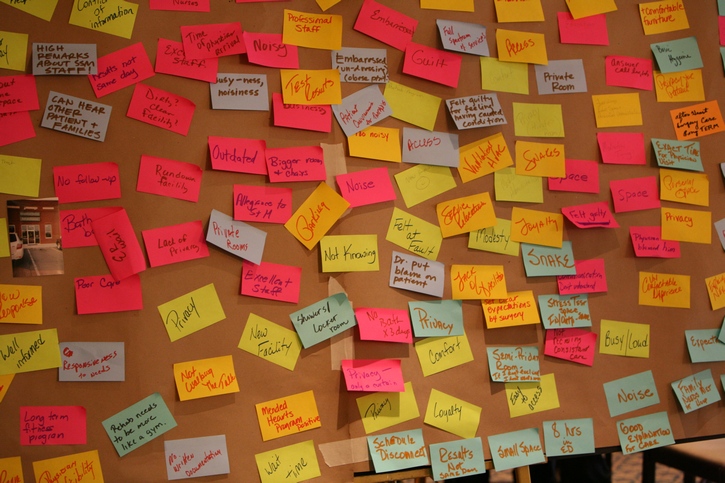
The collaborative model — a huge game-changer — is much more patient-centric. It’s based on a concept where everyone is aware of all aspects of the patient care. The endocrinologist is talking to the nutritionist to develop a program for the patient that eventually loops in the pharmacist for medication management, instead of relying on the patient to string all of the encounters together – now that’s powerful.
 The collaborative model trend also affects facility design and layout immensely. In order for 3-5 specialists to meet and develop programs for a patient, the space needs to be completely different. There needs to be open, larger collaborative spaces for this type of facility and healthcare treatment. Thus, it is moving further away from the typical “doctor’s office” and exam room layout.
The collaborative model trend also affects facility design and layout immensely. In order for 3-5 specialists to meet and develop programs for a patient, the space needs to be completely different. There needs to be open, larger collaborative spaces for this type of facility and healthcare treatment. Thus, it is moving further away from the typical “doctor’s office” and exam room layout.
It is a very different concept to have these open team spaces and a struggle to fit them into traditional MOBs. Optimally, it requires that they are located immediately adjacent to the encounter space to position the patient in the center of the care in close proximity with a care coordinator. The arrangement of spaces also must support the patient experience and workflow desired. It’s a deeper, richer experience that considers various aspects of care.
Below is a layout example. The blue represents the collaborative team spaces where specialists would meet.
This collaborative concept also stands to lower the cost per encounter (encounter would be considered a provider visit). With the diabetic patient example mentioned earlier, the individual appointments for each specialist holds a different cost per encounter. In a collaborative medical center where all the specialists are in one room, the cost per encounter is much lower even though the patient is still seeing all three specialists.
The collaborative, “patient-centered” concept is already present in many facilities across the nation. It’s just a matter of time before this specialty trend expands and becomes the normal process for healthcare in the United States.
Photos courtesy of HGA Architects and Engineers.
Author: Stan Chiu
Stan Chiu, AIA, LEED AP, is HGA’s healthcare principal. He has more than 20 years of experience in healthcare and higher education. He is a leader in Lean design and Integrated Project Delivery, and has helped develop core Lean IPD tools.
Tags: Architecture, Collaboration, Future Trends
Posted August 19, 2015
More Articles:
- State of Industry Examined in ‘Healthcare Reset’ Report
- Cam Twohey Joins Kahler Slater as Associate Principal, Senior Project Architect in Healthcare Market
- Perkins Eastman Welcomes Michael Hess as Principal in New York Studio
- Guerin Children’s Inpatient Pediatric Unit at Cedars-Sinai Provides Interactive, Family Friendly Healing Environment
- Coverings 2024
Apr 22, 2024 – Apr 25, 2024 - Hospital, Outpatient Facilities & Medical Office Buildings Summit
Apr 25, 2024 – Apr 25, 2024 - CxA Workshop & Exam
Apr 29, 2024 – Apr 30, 2024 - EMP Seminar & Exam at CxEnergy 2024
Apr 29, 2024 – Apr 30, 2024 - CxEnergy
Apr 29, 2024 – May 2, 2024 - PHCC West 2024
Apr 29, 2024 – May 2, 2024 - Lean in Design Forum 2024
May 1, 2024 – May 2, 2024