Comprehensive Flow Modeling
Over the past five or six years, many healthcare leaders have gained valuable insights from Building Information Modeling, for positive impacts on building design, construction and operation. Likewise, they have used energy modeling to improve building energy performance and sustainability. More recently, those leaders have made significant advances in the use of modeling and simulation technology, performing comprehensive utilization and flow models to envision and plan for the future and equally, or perhaps more importantly, to gain stakeholders’ support for incremental or even transformational change.

A Modeling Recap
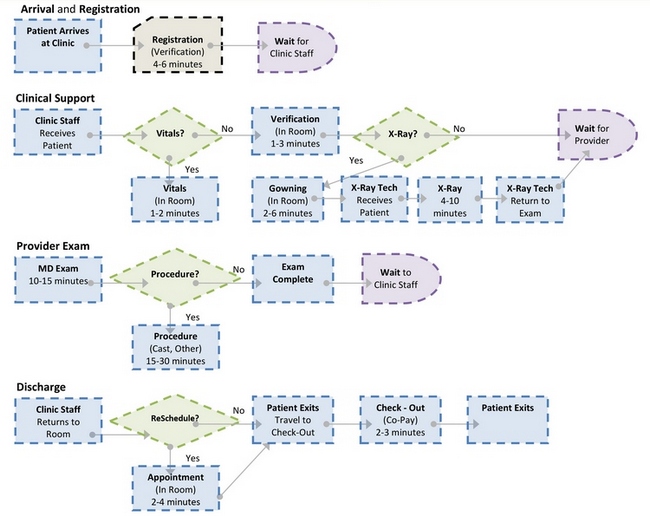
To briefly recap the concept of modeling, digital modeling technology (3-D and 5-D) enables visualization (3-D) of both healthcare facility design and operational variables, i.e., patient flow and provider/staff workflow; and, it quantifies (5-D) the effects of various alternatives in facility design and organizational processes on patient care and operational objectives.
The workflow modeling process starts with the creation of operational baselines and the identification of verifiable metrics that can be used to assess the effectiveness of alternative operational/design solutions. These comparisons of the present and future states in the virtual healthcare environment can become valuable leadership tools.
The 5-D models are developed by combining operational data (already gathered by most healthcare organizations), with operational projections or forecasts and various types of spatial representations, including floor plans, 3-D and 5-D facility simulation models and animations.
In essence, modeling enables us to create “virtual futures.”
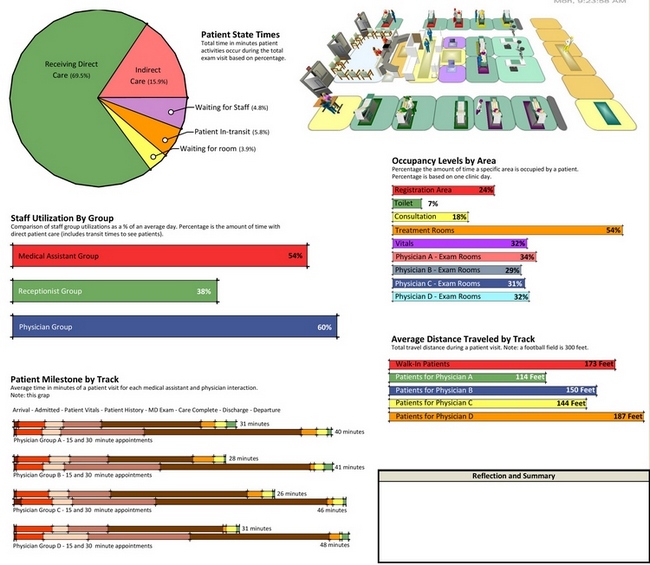
The Value to Leaders of Virtual Futures
Across a variety of patient-centered care projects from hospitals to community health centers to outpatient clinics, modeling of patient state times has driven innovations in workflow and design to significantly enhance the patient’s experience and satisfaction, while at the same time improving operational productivity. For example, if patients in a clinic spend 15 percent of their time engaged in activities that do not involve direct care from a physician or medical assistant, including filling out questionnaires and waiting for exam rooms and providers, the care team and project team can use wasted time metrics to explore and deploy alternatives in workflow and facility design.
Similarly, as we have gained the ability to simulate the effects of improved electronic digital communications and digital telemedicine in the healthcare business practice, formerly reluctant physician leaders have begun to embrace these technologies. When we can illustrate the fact that we don’t need an office because all the paperwork is going to be electronic, caregivers can visualize the use of a workstation to support electronic communications. When we can demonstrate in the virtual world how custom “apps” can be used to enable patients to navigate through the process of making online appointments using a tablet device, managers can see how this could streamline staffing, improve workflow and enhance patient satisfaction. When we illustrate and model a telemedicine conference room, with 3-D and 5-D tools, we can simulate the actual “telemedicine conference event,” leaders begin to experience the virtual future as an achievable reality.
Using Models to Enhance Planning
Once healthcare leaders have a model of the future, they can begin to formulate better plans for allocation of resources.
If we create a model based on demographic data that predicts a population boom in an area served by the healthcare system, then leaders can use the model to plan and recruit staff, expand the appropriate facilities and adjust processes to increase capacity.
Similarly, if the healthcare industry anticipates significant advancements in diagnostic technology, leaders can use models to modify facilities to better utilize those technologies, recruit and train staff, prepare patients and ready their organization for those coming changes.
Knowing the needs and expectations of patients have changed dramatically with respect to hours of access, many healthcare organizations are expanding their hours of service. A model of this future state can enable leaders to mobilize, assign resources and establish priorities in order to meet those patient needs and expectations. Historically, traditional outpatient offices and clinics were open roughly 8 a.m. to 5 p.m. With the emergence in the healthcare market of urgent care or convenient care facilities and data that monitors hours of operation, patient utilization and financial results, traditional healthcare organizations are embracing innovations that allow for more flexible hours.
Using Working Sessions to Illuminate Data
Working sessions involving the project team and healthcare leaders in modeling can be used quite effectively to illuminate data. When working with a capacity forecast, we have used flow models and the video associated with the simulation to illustrate that, at certain times of the day, there will be events causing congestion or reflecting lack of capacity. Specifically, the model extrapolates data from the simulation to provide evidence that given certain rates of speed (of care delivery) and rates of utilization, the facility will have a shortage or an excess of resources. In turn, the project team and leaders can also discuss and model the effects of facility design and/or process changes to improve flow.
In fact, flow management is fairly difficult to appreciate without a simulation model. In order to develop an effective scheduling strategy, leaders and providers must understand what is happening with flow. Just as with BIM, flow modeling has become a valuable tool enhancing the ability to predict and enact necessary change for better outcomes.
For example, flow modeling depicts which workflow processes in the surgery department are causing delays in the OR turn-over rate, with a resultant loss of capacity. The same type of metric generation applies to forecasting and planning for improvements in flow relative to increased capacity in diagnostic imaging.
Staff utilization benchmarks provide another dramatic example. The national average physician-patient contact time for primary care is eight minutes. Theoretically, without a lot of effort, a provider should be able to see five patients in 40 minutes, allowing a total of 20 minutes per hour of collateral time between patients. In total, a provider should be able to see 40 patients a day. Yet the national productivity average is only 25 patients a day. This objective analysis of how effectively and efficiently time is allocated is very powerful. Once leaders obtain modeling and simulation data for their organization, they can enable better decisions regarding staff and resource utilization.



